During the past 50 years, the U.S. has led an international movement in palliative care, dedicated to improving the lives of patients with painful or debilitating illnesses such as heart failure, chronic obstructive lung disease (COPD), cancer, HIV/AIDS, cirrhosis, kidney disease and degenerative nervous system diseases like dementia.
Yet many Americans are either unfamiliar with the term “palliative care” or think it’s only part of end-of-life care.
It is important to spread the word that palliative care should be, and often is, integrated into the very beginning of treatment for painful or discomforting illnesses. While palliative care does not cure such illnesses, it enables patients and their families to have a better quality of life from the time of diagnosis forward.
Palliative care is becoming a major component of health care reform because it enhances quality care and reduces the cost of health care.
Palliative care is a model of care — a therapeutic approach — dedicated to reducing “illness burden” and suffering of the patient and the family.
In the U.S., there are two broad types of palliative care. Generalist-level palliative care is a best practice that can be employed by all health professionals. Specialist-level palliative care is provided by professionals — physicians, nurses, social workers and chaplains — with advanced training and skills who work as a team to create a palliative plan of care.
Generalist-level treatments and services can be managed by the primary physician. If problems become complex or difficult to manage, this physician should discuss with the patient a referral to a palliative care specialist.
Palliative care addresses an array of problems divided into eight so-called “domains.” Specialist-level palliative care programs address all of these domains:
n Physical well-being. Treatments relieve pain along with other symptoms or manage other physical problems.
n Psychological well-being. Support is offered to help the patient adapt to the disease or to relieve anxiety, depression or other psychological problems.
n Social well-being. Efforts target the family and help the patient remain connected to others.
n Spiritual well-being. Care helps the patient and family deal with a loss of purpose or meaning as well as with religious concerns.
n Structures and processes of good care. Patients and families are involved in discussing treatment risks and benefits, prognosis and goals as well as decision-making. The system of care may change to provide better services and support consistency of care.
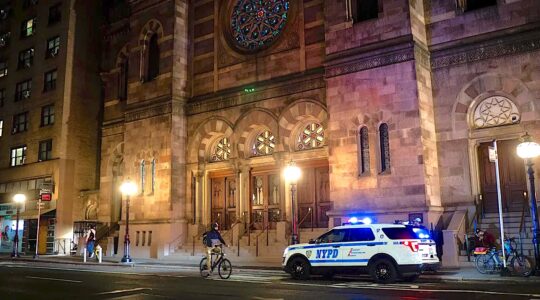
Support the New York Jewish Week
Our nonprofit newsroom depends on readers like you. Make a donation now to support independent Jewish journalism in New York.
n Cultural aspects of good care. Treatment plans focus on the need to respect cultural values.
n Legal and ethical aspects of good care. Challenging decisions, such as whether to stop a medicine when the benefit is minimal, are examined and informed by knowledge of the law and ethics.
n Care of the imminently dying. If death appears to be soon, the goals may shift to treatments that ensure a comfortable and dignified death, while providing support for the family.
In the U.S., hospice is a benefit provided by Medicare, Medicaid and many private insurance policies. It offers excellent palliative care for individuals with advanced, life-limiting illnesses. Typically, patients are considered for hospice referral when life expectancy is considered to be less than six months. The hospice team usually visits patients in the home or nursing home, and provides comprehensive end-of-life care.
Research studies have shown that palliative care enhances quality of care and reduces overall health care costs by involving patients in making informed decisions about their own care.
Today, most hospitals have palliative care programs. In the coming decade, community-based palliative care programs, such as those developed by New York’s MJHS Hospice and Palliative Care, will take the lead in coordinating with hospital programs and with hospice to benefit patients and families and the broader health care system.
Dr. Russell Portenoy is chief medical officer for MJHS Hospice and Palliative Care, professor of neurology and anesthesiology at the Albert Einstein College of Medicine and editor of Journal of Pain and Symptom Management. He can be reached at rporteno@mjhs.org.
The New York Jewish Week brings you the stories behind the headlines, keeping you connected to Jewish life in New York. Help sustain the reporting you trust by donating today.